Research in the Meng Lab focuses on the following:
Kidney Cancer
The number of patients diagnosed with kidney cancer has risen in recent years due to increased usage of imaging such as ultrasound, CT or MRI scans for other clinical reasons. This has led to the discovery of many small kidney tumors which may simply be observed given their indolent nature. However, a portion of these small kidney tumors can grow rapidly and spread to other parts of the body. The diagnostic dilemma is separating out which tumors may need treatment from those that can be safely watched.
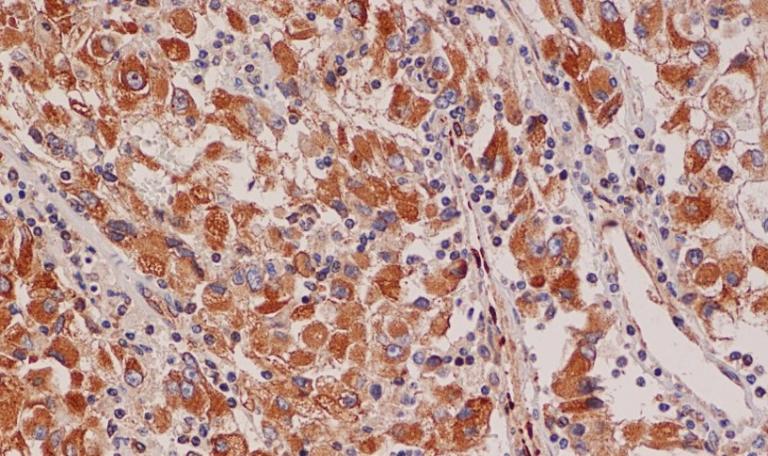
To better understand the process of tumor invasion in kidney cancer, we are working on a project to examine how cell polarity proteins are altered in kidney tumors. This group of proteins regulate the orientation of cells, a process disrupted in invasive tumors, and have been shown to play a key role in multiple other cancers such as liver and breast cancer.
We are examining arrays of patient kidney tumor samples to better understand how these changes to cell polarity proteins are different in localized versus invasive kidney tumors. In addition to our work with patient samples, we are also embarking on molecular studies focused on the role of the Par complex in primary versus metastatic kidney cancer cell lines. We are examining the localization, protein levels and interactors with these critical cell polarity complex proteins in multiple kidney cancer cell lines to understand their role in development of invasive disease.
Our goal is that these projects in conjunction will provide greater insight on the significance of cell polarity alterations and how it contributes to the development of invasive disease in kidney cancer. A deeper understanding of these fundamental processes will help us better develop new diagnostic tests and models to help differentiating between indolent vs. invasive tumors. In the short term, this data could be utilized clinically to improve the diagnostic utility of renal biopsy and lead to development of predictive models for selecting patients with aggressive tumors for clinical trials. Ultimately, this could lead to tailored treatment options based on the aggressiveness of tumors, decreasing the morbidity of overtreatment, preserving long term renal function, and limiting the risk of developing metastatic disease.
Focal Therapy in Prostate Cancer
Prostate cancer is one of the most frequently diagnosed cancers and a leading cause of death in men, yet the diverse spectrum of prostate cancer, ranging from indolent to aggressive disease, creates many challenges for determining the optimal treatment for each man. While treatment such as surgery or radiation for low to intermediate risk prostate cancer yields excellent prognosis, it may lead to overtreatment for patients, resulting in significant long term side effects including urinary incontinence, erectile dysfunction and other long-term complications such urinary and rectal infections, bleeding, recto-urethral fistulas and secondary malignancies. Patients with low grade prostate cancer are ideal for being on active surveillance, but eventually half of these men will elect for radical, in part due to diagnostic uncertainly of occult higher-grade prostate cancer and the ongoing worry about living with an active malignancy.
Focal therapy represents the middle ground between active surveillance and radical treatment and is widely used for other malignancies such as thyroid, liver, breast, and brain cancer. Focal therapy for prostate cancer involves targeting individual areas of cancer while preserving the remaining prostate tissue and critical surrounding structures such as the neurovascular bundles and bladder neck, offer an appealing alternative to radical therapy, with potential benefits of a relatively non-morbid intervention and cancer eradication. However, the current downside of focal therapy is the higher rates of cancer recurrence compared to surgery and radiation, in part due to the lack of a clear definition of the optimal focal therapy candidate. For focal therapy to be a successful long-term treatment modality for prostate cancer, optimizing patient selection and identifying potential avenues of treatment failure are of critical importance.
To address this problem of which prostate cancer patients are best served by focal therapy, we propose a comprehensive analysis of clinical factors involved in identifying candidates for focal therapy, as well as translational correlates focusing on the tumor microenvironment and imaging changes due to focal ablation. While we currently consider intermediate risk men to be the best focal therapy candidates, this broad characterization based primarily on clinical staging, Gleason score and PSA is not sufficiently detailed enough to account for variations in tumor location, relationship to critical structures and potential extra-capsular disease that would be identified on prostate imaging. Moreover, given the considerable racial disparity in the incidence and mortality rates of prostate cancer in the U.S., additional factors outside of traditional clinical data may need to be considered when offering a patient focal therapy.
By critically evaluating all these factors, we expect to develop a patient selection algorithm that identifies tumor characteristics that are likely to result in failure of focal therapy. This will ultimately enable us to selectively treat prostate cancer patients that respond best to focal therapy without sacrificing oncologic control.