Mitochondrial stress, immune signaling, and autoinflammatory diseases
Emerging evidence suggests that mitochondria serve as a signaling hub in immune cells that converts signals from inflammatory insults (e.g. pathogenic and/or self-derived stimuli) into immunological output (e.g. immune activation, tolerance, and resistance). We are interested in understanding how mitochondria sense the perturbation of immune homeostasis and how they respond to such events. By delineating the molecular mechanisms involved, we aim at comprehensively investigating the role of mitochondria in immune signaling in the context of autoinflammatory diseases.
 Mitochondrion
Mitochondrion 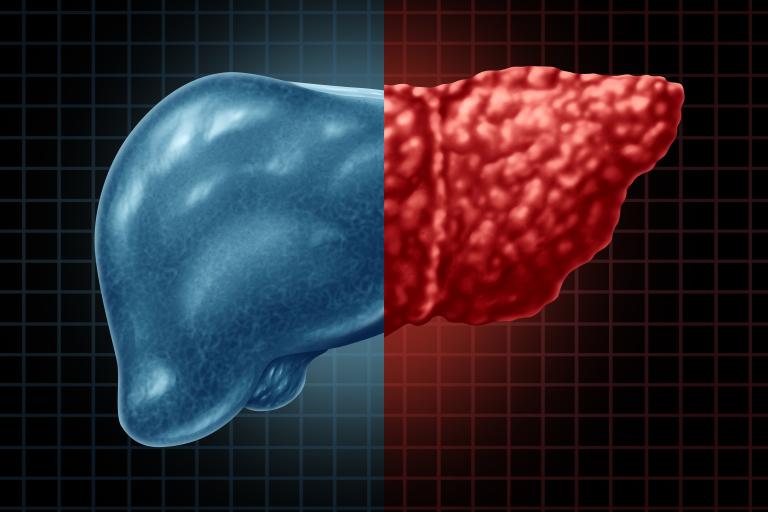 Diseased liver
Diseased liver Obesity-Associated Liver Diseases
With the unprecedented obesity epidemic, nonalcoholic steatohepatitis (NASH) now becomes a major chronic liver disorder, affecting 3-5% of the global population. NASH is an advanced form of nonalcoholic fatty liver disease (NAFLD)—a spectrum of chronic liver disorders that originate from benign fatty liver (simple steatosis) that can further progress into NASH, cirrhosis and even hepatocellular carcinoma (HCC). It is well-established that chronic liver inflammation is the key switch that drives simple steatosis transition into NASH. However, how dietary obesity licenses the establishment of chronic inflammation in the liver remains elusive. We aim to uncover the fundamental mechanisms by which chronic liver inflammation is established in the liver under obesity. By deploying a combination of biochemical, genetic, molecular, immunological, imaging, and histochemical tools as well as single-cell “omics” analyses, our ultimate goal is to reveal the fundamental molecular mechanisms underlying chronic liver inflammation and explore if such novel mechanistic insights could be applied to benefit liver repair and regeneration processes after injury, thereby preventing NAFLD progression into NASH/HCC.
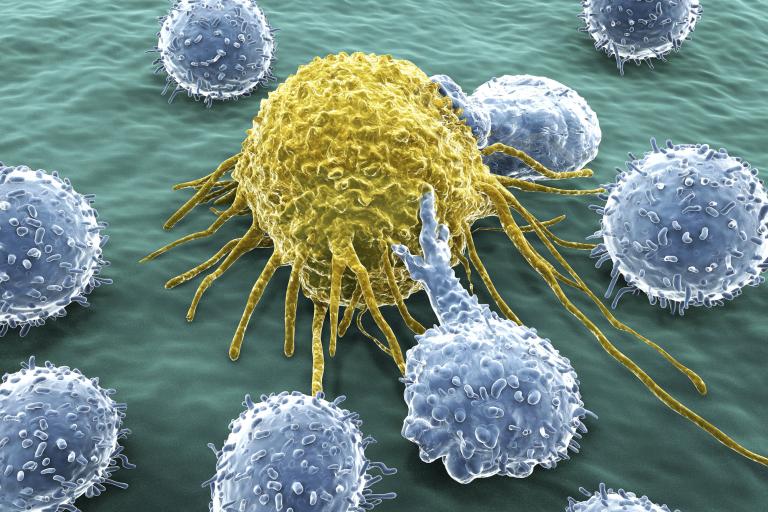
Cancer Innate Immune Therapy
The discovery of immune checkpoints in T cell activation has revolutionized anti-cancer treatment strategies. Cancer immunotherapy has achieved unprecedented success in cancer patients who respond to such therapies. However, among those “non-responders”, in which the tumors are usually described as “cold” or “desert”, it remains challenging to induce potent and tumor antigen-specific adaptive immunities—a fact that is at least partially due to inefficient innate immune activation by tumor cells. Our goal is to develop strategies that modulate host innate immune system and thereby induce potent yet transient innate immune activation in the tumor microenvironment to ultimately turn a “cold” tumor into a “hot” one. We believe that such cancer innate immune therapy would help overcome resistance to immune checkpoint blockade strategies.
 Macrophages
Macrophages