Laboratory of Tissue Immunity and Host-Microbe Interactions
In the company of Microbes, all small things are considered
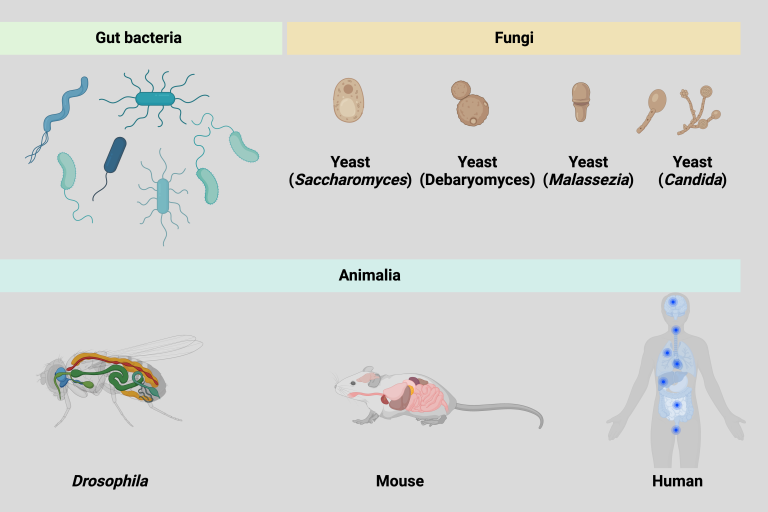
The microbiome plays an essential role in modulating host immune responses, in the setting of health and disease. The mycobiome, the fungal microbiota, is an essential but overlooked aspect of the gut microbiome. Exploring fundamental mechanisms of how commensal fungi survive and persist within a host niche filled with a multitude of innate and adaptive immune effectors will not only provide unique insight into human diseases (such as IBD and cancer) but also could provide the foundation for novel immunotherapy therapeutic approaches.
Yeasts (eukaryotic, single-celled microorganisms classified within the fungal kingdom), such as Candida species and Saccharomyces spp, dominate the human mycobiota. Human commensal Candida, exhibit significant immunoreactive properties when interacting with host immunity in the gut. Candida can produce specific fungal protein effectors, such as candidalysin, adhesins, or potentially unknown factors, that induce both innate and adaptive immune responses. However, some important questions remain to be addressed. Overall, our lab is interested in exploring future directions to understand how tissue immunity evolves, initiates, and orchestrates by addressing several key questions.
How do commensal fungi interact with host immunity during homeostasis and diseases?
The innate immune system detects microbes using pattern recognition receptors (PRRs) encoded in the germline. These PRRs detect conserved microbial structures termed pathogen-associated molecular patterns (PAMPs), giving rise to PAMP-triggered immunity. Beyond PAMPs, there's a distinct immune response defined as effector triggered immunity. Originating from plant research and later adapted to metazoans, ETI is an immune response activated by virulence/protein-associated activities of pathogens. Effector proteins include any microbial protein molecule, such as enzymes or even broad categories like toxins, which modulate the host's immune activation.
What are the ideal experimental model systems to understand the interactions between commensal fungi and the host?
Our study has illustrated that gut-isolated human commensal species, exhibits marked genetic diversity within the human gastrointestinal tract. While exploring strain variations in bacteria and viruses have advanced, comparable studies in fungal strains are essentially lagging, largely due to the complexity of its diploid nature and the lack of tractable genetic tools. These observations highlight the urgent need to develop effective genetic tools for studying human gut-derived fungi. Such advancements will significantly foster discoveries in microbial biology and host-microbe intestinal immunity.
Can we harness the unique features of commensal fungi and host interactions toward a therapeutic platform? Our aim is to leverage the unique features of commensal fungi and host interactions to advance the treatment of inflammatory diseases. We will use genetic engineering to develop new therapeutic approaches for antigen delivery. We can precisely modulate this aspect to enhance antigen delivery while still considering the potential pathogenicity associated with fungi.
Our lab aims to identify new microbial effectors and host determinants involved in fungal and bacterial sensing through interdisciplinary approaches, such as CRISPR-based genetic editing, in vitro screening, animal models, and human patient resources. This research will contribute to regulating immune homeostasis and preventing inflammatory diseases.