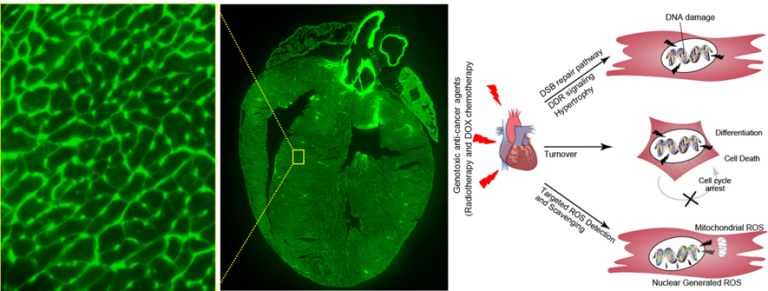
Cancer now affects more than one in three people in their lifetime and, along with cardiovascular disease, they are the two leading causes of death in developed nations. Overall 10-year cancer survival stands at 50% across the 20 most common malignancies and approximately 80% or better in breast, lymphoma, melanoma, and uterine cancers. These mortality trends reflect a broad improvement in survival rates in developed economies. Cancer outcomes continue to improve due to earlier detection and newer targeted therapies, with anthracycline chemotherapy and chest radiotherapy, playing a major role in the modern era of cancer treatment. Paradoxically, improved long-term cancer survival has led to increased adverse cardiac effects of cancer treatment itself. Due to this paradigm shift from cancer survival to cancer survivorship, we require a better understanding of the mechanism by which the genotoxic cancer therapeutics initiate long-lasting adverse effects on cardiomyocyte.
 Radiotherapy/chemotherapy and heart damage
Radiotherapy/chemotherapy and heart damage Radiation therapy is one of the primary modalities for the treatment of many cancers, including chest malignancies such as lung cancer and esophageal cancer. It has been estimated that nearly 50% of all cancer patients receive therapeutic radiation as a component of their treatment. Consequently, radiation-induced cardiac injury is a significant contributor to cardiovascular disease-related mortality in the United States and around the world. Consistent with this, studies have shown that a significant proportion of patients receiving definitive radiation therapy for non-small cell lung cancer (NSCLC) experienced cardiac events within two to five years after the completion of radiotherapy. With improvements in systemic therapies, including the advent of immunotherapies, the long-term survival in patients with lung cancer and thoracic malignancies is improving and radiation-induced heart disease (RIHD) remains a major source of morbidity and mortality in such patients. Therefore, there is an urgent need to study the molecular mechanisms underlying radiation-induced heart disease.
Cancer therapy with anthracycline, including doxorubicin (DOX), regimens plays a prominent role in many cancer treatments. For example, 32% of breast cancer patients, 57–70% of elderly lymphoma patients, and 50–60% of childhood cancer survivors are treated with an anthracycline regimen. Paradoxically, anthracycline remains a leading cause of cardiovascular morbidity and mortality after cancer treatment, particularly when used in combination with chest radiation therapy. Doxorubicin exerts its cytotoxic effect by intercalating DNA. Doxorubicin binds with DNA and topoisomerase 2 isoenzymes forming a ternary Top2-doxorubicin-DNA complex, which causes double-stranded DNA breaks (DSBs). When bound to Top2α, the complex inhibits DNA replication; arrests the cell cycle in G1/G2; and induces apoptosis as intended in proliferating malignant cells. Conversely, when bound to Top2β, mitochondrial dysfunction is triggered by the suppression of the peroxisome proliferator-activated receptor, which regulates oxidative metabolism. Thus, DOX exerts its effect on all cardiomyocytes via ROS and may act as well by preventing the proliferation of cycling cardiomyocytes. Yet, from a mechanistic standpoint, the downstream effects of DOX-induced DNA damage in cardiomyocytes and the specific DSB repair and DDR signaling that are activated in cardiomyocytes following DOX-induced DNA damage are unknown.
Our group studies the effect of cancer therapeutics and aging on the growth and renewal of heart muscle. We investigate how to prevent the deleterious effects of cancer therapeutics and aging-associated effects on cardiomyocytes and develop countermeasures for minimizing, preventing, or reversing both therapeutic-induced and aging-related myocardial damage using a wide variety of transgenic mice models.