What is Prematurity?
For humans, a full-term pregnancy lasts 40 weeks (about 9 months). A way to track a baby’s growth is through gestational age, which is a fancy way of saying the number of weeks and days spent inside a mother’s belly.
Each person has a different story to share about how they were born:
- Full-term babies are born right around 37-40 weeks, when their body has fully grown and is ready to come out into the world.
- Babies born more than 3 weeks before their expected due date are called “premature.” Premature babies (also called preemies) may not have enough time to grow and develop as much as they should have before birth.
- Very to extremely premature babies can come a lot earlier than expected at around 23-32 weeks. Doctors and nurses can help these preemies by giving care to them in a neonatal intensive care unit (NICU).
Babies that are born earlier than expected are so common that 1 in 10 babies are born prematurely. Since premature babies had less time to grow, that means that their heart and lungs may not work the same way as full-term babies. Luckily, medicine and research can help us understand what and how these differences end up playing a role in the babies’ life.

What is the CAPE Study?
The Cardiac Growth After PrEterm Birth study (also known as the CAPE study) is a research study at UT Southwestern, Parkland Hospital, and Children’s Health that helps doctors and scientists understand and compare how the heart and lungs develop in both babies born very to extremely premature (23-32 weeks) to those who were born at term (37 weeks-40+ weeks).
We are looking for participants between ages 8 and 30 who were born prematurely or born at term.
If you decide to participate or have your child participate in this research study, the research team will ask you to complete a study visit on Year 1, and another 2 years later (Year 3).
During each study visit, there will be questionnaires regarding patient health history, measures such as height, weight, vital signs (heart rate and blood pressure), biospecimen collection (such as blood and urine) and tests to measure lung and heart function.
We will measure lung and heart function through 3 procedures:
1. Echocardiogram (ECHO)
An echocardiogram (also called an echo or cardiac ultrasound) uses sound waves to create pictures of the heart. This painless ultrasound test shows the structure of the heart and its parts and how well they’re working. This can help look for any problems with the heart’s walls and valves, the blood vessels leading to and from the heart, and the heart’s pumping strength.
An echocardiogram is done in a darkened room, while you are lying down. Small stickers (called electrodes) are placed on your chest. These measure the rhythm of your heart beating. Gel put on your chest helps sound waves travel from the echocardiogram wand to the heart and back again. The person doing the test will move the wand around to get pictures of the heart from different angles. This usually takes 30-60 minutes to get the pictures needed.
2. Pulmonary Function Test (PFT)
Lung (or pulmonary) function tests are a variety of tests that measure how well a person breathes. One example of a lung function test is called spirometry, which involves breathing into a tube that records how much and how quickly air can be breathed out following a deep breath in. This can take 15-45 minutes to complete.
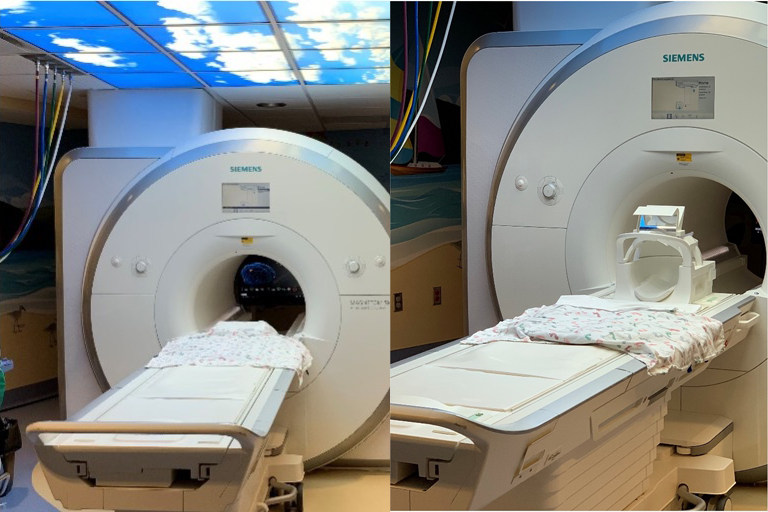
3. Cardiac MRI
A cardiac MRI (magnetic resonance imaging) scan creates detailed pictures of your heart. The test is painless, and you must hold very still so the pictures come out clear. The person taking your pictures (MRI tech) will ask you to hold your breath for several seconds at a time. This will take 45-75 minutes to complete. Note: You will have the option to watch a movie during the scan.
Because the MRI machine uses strong magnets, you will have to take off anything metal like jewelry, watches, or glasses.
At right is a picture of an MRI scanner, which looks like a tunnel. This will be the camera we will use to take your pictures!
Sometimes, you might need to get something called contrast, given through an IV. This will help doctors see your heart better.
What is an IV?
An IV is a medicine straw that can be used to give you medicine or draw blood if needed.
IVs are mostly placed in your veins in your hand or arm. There is a small needle that helps get the IV straw to the right spot of your vein, but the needle comes out so just the straw stays in place. The nurse can give you numbing medicine to help you feel the poke less. The IV will be removed after your MRI is complete.






