While mortality rates for critically ill patients suffering from trauma, sepsis, and burn injury have significantly declined, many patients progress to a state of chronic critical illness, requiring ICU stays of weeks to months. The recovery period for these ICU survivors is often fraught with multiple complications, substantial disability, and long-term neurocognitive deficits.
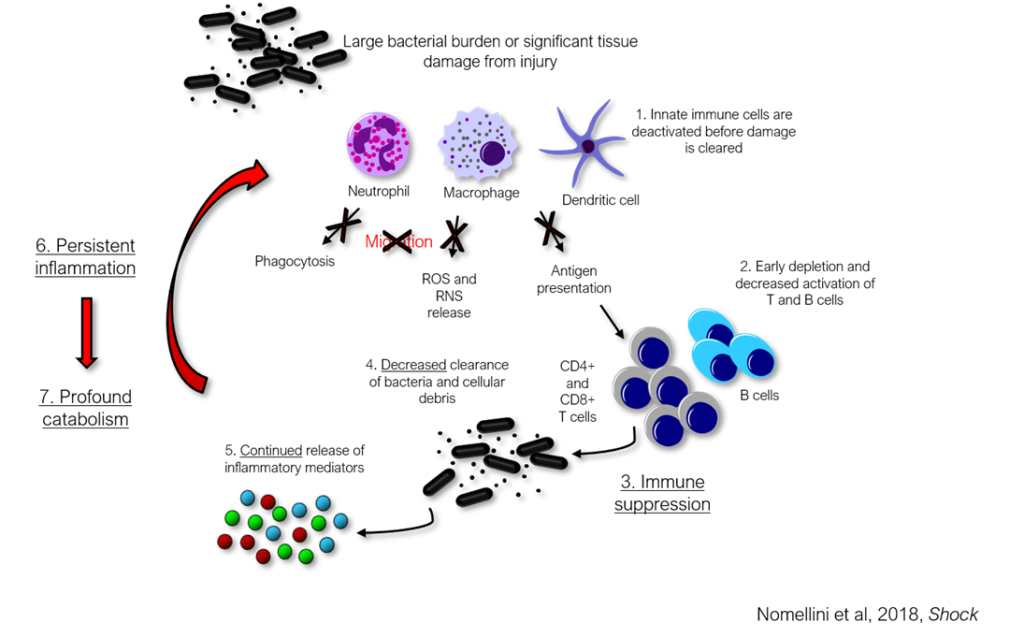
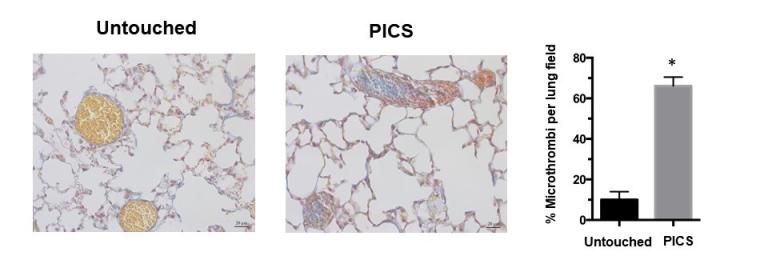
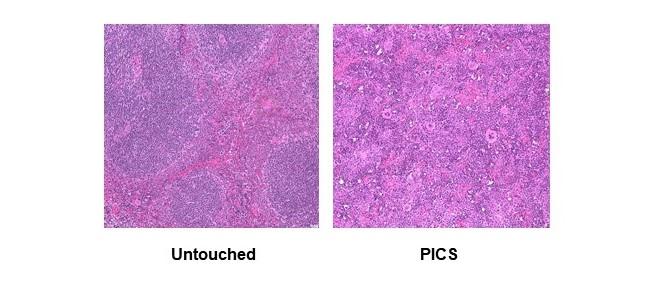
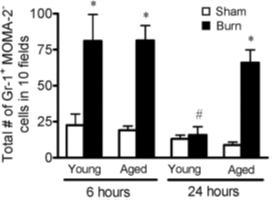
The main risk factor for the development of chronic critical illness is the degree of immunosuppression that can occur. Another term for this state is the Persistent Inflammation, Immunosuppression, and Catabolism Syndrome (PICS). The theory behind PICS is that, when there is a significant burden of invading bacteria and/or a substantial amount of tissue injury, the immune system becomes overwhelmed. This then leads to global suppression of the immune response, with changes seen in both the first line of defense against invading pathogens (the innate immune system) and the more advanced, pathogen-specific response (the adaptive immune system). Many have been able to show this immunosuppressed state in critically ill patients, but no one has been able to reverse this response.
Our lab examines: 1) the interaction between the innate and adaptive immune responses that occur after injury or infection, and 2) the heterogeneity of the immune responses that occur in each individual to develop personalized immune therapies to reverse the immunosuppression that can occur in ICU survivors. Ultimately, we hope to minimize the development of chronic critical illness and improve the outcomes of this complex patient population.